How to Heal the Gut After Antibiotics

Perhaps you or your child recently finished a round and want to know how to heal the gut after antibiotics. You’re in the right spot!
But first, are antibiotics really necessary?
I often get asked about my take on antibiotics. And it’s simply not black and white. Are they massively over-prescribed? In my opinion, yes. Are they lifesaving and sometimes necessary? Also, yes. I believe antibiotics should be used as a last option instead of the first course of action. I’m all for lifestyle interventions and supplementation before antibiotics in order to fight bugs and beat sickness!
What’s wrong with antibiotics?
While antibiotics are a powerful medicine effective at fighting off unwanted bacteria and overcoming certain infections and illnesses, they have a big downside. Not only do antibiotics wipe out all of the harmful bugs, they wipe out our beneficial bacteria as well.
That ultimately means decreased immunity, greater susceptibility to unwanted gut pathogens, increased likelihood for gut dysbiosis, and a higher chance of all of the unwanted symptoms that go along with those things – digestive distress, stomach pain, constipation, and/or diarrhea, cramps, and more.
Additionally, over-usage of antibiotics can cause you to become more vulnerable to “superbugs.” Essentially, bacteria “morph” to multiply faster and become more difficult to kill. In my blog post Are Antibiotics Causing More Harm Than Good?, you can learn more about the powerfully negative effects of antibiotics.
But what happens if you really need to take antibiotics?
Sometimes antibiotics are necessary. It’s an unfortunate reality that many of us know. While it helps to know beforehand that your gut may experience unwanted symptoms and discomfort, this is not the time to panic. Instead, I want you to focus on what you can do to restore strength to your gut microbiome.
I’m going to give you some tips and tricks and a solid plan to get your gut back on track after antibiotics do their thing.
How to restore gut health after taking antibiotics:
1. Increase the diversity of foods in your diet. Eat the rainbow!
Especially when attempting to repopulate the gut with beneficial bacteria, it’s highly advised to eat a rich variety of healthy, whole foods. In fact, links have been found between diverse gut microbiomes and healthy dietary patterns, including high-fiber vegetables and clean animal proteins such as eggs and fish. For that reason and more, I encourage my post-antibiotic clients to eat as many colorful real foods as possible.
It makes sense, right? The more real, whole and healthy foods you “feed” the good bacteria, the more robust and diversified they will become!
2. Eat a gut-healing + nutrient-dense diet. Go low/no sugar, alcohol or processed food.
To rehabilitate the gut after antibiotic usage, a focus on gut healing and nutrient-dense foods is crucial. Additionally, cutting out sugars and processed foods is equally important.
Why is cutting sugar important? Because sugar feeds pro-inflammatory bacteria in the gut such as Proteobacteria. It also makes you more susceptible to Candida overgrowth. If you’re taking antibiotics, you’re already at a higher risk for Candida, other fungal overgrowth and dysbiosis. A diet that is even moderate to high in sugar only furthers the risk for these things post-antibiotics.
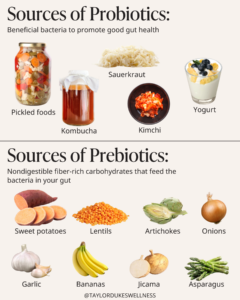
Gut-healing and nutrient-dense foods that soothe the gut lining, feed the good bugs, decrease inflammation, and promote microbiome health will include a mix of prebiotic and probiotic-rich foods along with foods that contain collagen, amino acids, and gelatin.
A collagen and gelatin-rich hero is bone broth, and it should absolutely be part of any post-antibiotic diet. Other fantastic and soothing foods include wild-caught fish, chamomile tea, aloe vera, full-fat coconut products, and plenty of cooked organic veggies.
I always point clients toward my Gut Healing Green Soup, and there’s never a better time to have it multiple times a week than post-antibiotics.
3. Focus on a gut-supportive supplement plan, including prebiotics and probiotics.
I highly suggest gut-supportive supplements if you must take antibiotics.
This is my recommendation for any of my clients while taking antibiotics:
- High-quality prebiotic (1 capsule/day)
- Saccharomyces Boulardii (1 capsule/day)
This is my recommendation for a minimum of 60 days post-antibiotic:
- Tier One: These are the supplements that I absolutely advise for any of my clients post-antibiotic.
- High-quality prebiotic (1 capsule/day)
- High-quality probiotic* (1 capsule/day)
- Saccharomyces Boulardii (1 capsule/day)
- Tier Two: These are the “icing on the cake” supplements that will expedite healing and optimize gut wellness post-antibiotic.
- GI Immune Support** (1 scoop daily)
- Gut Support** (1 scoop daily)
- Note that as an option, you can do 60 days of all aforementioned supplements, or you can do 60 days of Tier 1 followed by 60 days of Tier 2 supplements.
*Ensure that your high-quality probiotic has a variety of strains to diversify your gut as much as possible. It should have different strains of Lactobacilli, Bifidobacteria or Saccharomyces Boulardii. If it does have Saccharomyces Boulardii, it is not necessary to take additional, but it won’t cause harm and only help if you do. And always make sure you’re taking your probiotic at least two hours away from the antibiotic. You can read my previous articles on why you should be taking prebiotics AND probiotics.
**GI Immune Support is a dairy-free alternative to colostrum, and it is great for post-antibiotics since it eliminates pathogens from the gut. Gut Support also strengthens the gut lining, decreases gut inflammation, and provides concentrated nutrition for gut cells.
***Note that for children, I generally recommend the same type of protocol. You can use Clark’s Rule to determine pediatric dosing. I have great options for children’s supplements on my Fullscript. I personally prioritize GI Immune Support powder for my children because it is so effective and easy to administer as it’s a powder!!
4. Consider an anti-fungal supplement.
Some people are very prone to having Candida or yeast overgrowth, and this is particularly the case post-antibiotics. The reason is, antibiotics kill off the beneficial bacteria that would otherwise normally keep Candida in check.
For this reason, you may want to consider anti-fungal supplements like Clean – available in liquid and capsules. It is formulated with 18 botanical extracts and essential oils that detox the entire GI tract of harmful parasites, bacteria, Candida, and other yeast/fungus while selectively enhancing beneficial organisms.
For more information on how to be tested for fungal markers and to receive my recommendations for supplements such as those mentioned above, keep reading to #7 below. You may be the perfect candidate for stool testing and my gut program, which I offer exclusively through TDW Community!
5. Movement for the gut-supportive benefits.
Research shows exercise can positively impact your gut microbiome health by increasing beneficial microorganisms. Another study showed that women who participated in regular aerobic exercise for just 3 hours a week had increased levels of good gut bacteria.
Now get your workout shoes on and get outside…even if your lugging the kiddos along in the stroller!
6. Relax and destress (without a glass of wine, sorry!)
Stress itself can damage the gut through stress hormones, inflammation and autonomic alterations. Acute and chronic stress were found to promote harmful bacteria, which prolongs the time it takes to heal your gut after antibiotics.
If you want to successfully replenish beneficial gut bacteria, then you’ll need to manage your stress well. It’s unrealistic to think that stress won’t happen. It’s a natural part of life for everyone! It’s what you do with your stress and how you deal with it that can either make you more resilient or slowly deteriorate your health.
Stress reduction measures can include gentle movement, time outdoors, time spent with loved ones, sleep, journaling, reading, counseling, or whatever else happens to speak to you.
A quick side note…when you are de-stressing, do it sans the wine. Research shows that excessive alcohol can encourage bad bacteria to populate while reducing good bacteria.
7. Get help from a functional medicine perspective.
If you are still having gut issues or other symptoms after antibiotics, please reach out to a functional healthcare provider. Stool testing may be your best move to really understand what’s going on inside the gut. Gut health can be tricky, and stool testing (along with other tests, possibly) allows for clear insight and a plan.
Even if two people were on the same antibiotic at the same time, they may have differences in strains of bacteria and bacterial levels, digestive symptoms, and inflammation markers. Measures to improve your gut health truly must be personalized.
If you’re interested in a stool test, a personalized protocol based on the results, and the opportunity to meet with an experienced provider on my team, then look no further than The TDW Community. Through my Community, you will gain access best in functional medicine GI-Map stool testing, access to me and my team, and my entire Get Your Gut Right Program, which has helped hundreds of people alleviate unwanted symptoms and experience the joy of well-being!
How long does it take to restore the gut after antibiotics?
Finally, what everyone wants to know – How long does it take to heal the gut?! I don’t want to disappoint you, but it takes some time! This length of time will be different based on each person’s bio-individuality as well as the length of the measures they take to heal the gut. This is why I recommend avoiding antibiotics in the first place unless they are necessary.
In general, I recommend allowing for at least 6 months for your gut to fully recover. But don’t underestimate the power of healthy lifestyle choices to quicken your recovery. If you truly focus on the measures given above, trust that you’re giving yourself your best bet to heal as quickly as possible.
Whether through supplements, my comprehensive gut program available through TDW Community, or simply all of the free education on my blog and Instagram, I’m here to support you in your journey to better health!
Share This Post:
Your Wellness Deep Dive
- Be the first to learn about new healthy living resources, blog posts, and exclusive TDW offerings by getting on my insider list.
- Find healthy living products with ingredients you can trust – the same ones I personally use for myself and my family – in the TDW Shop. Check out our protein powders, electrolytes, supplements, and more!
- Get personalized support through the TDW Community. When you become a member, you get access to functional medicine expertise from me and my team, functional medicine lab testing and 1:1 consults, a digital library of exclusive wellness content, live monthly Q&As with me, and so much more!
YOU MAY ALSO LIKE:
Helping you get your gut right, improve energy, boost immunity, balance hormones, sleep better and look + feel your best
DISCLAIMER
PRIVACY POLICY
TERMS + CONDITIONS
ACCESSIBILITY
© 2025 Taylor Dukes Wellness
LEARN
SHOP
ABOUT
TDW Community
Free Guides
Blog
TDW Store
Fullscript
About Taylor
Press
Contact
COOKIE POLICY
SITE CREDIT
Trusted Products



